
What are we missing here in Ontario in building innovative care models to scale?
Following our roundtable event held in September, this article details the contents and outcomes of our discussion on fostering innovations in senior care.
Background
Ontario’s struggle to care for its seniors
It’s not news that as we age, we need more care. Consequently, a disproportionate fraction of our healthcare system is focused on caring for our seniors. Ontarians over the age of 60 account for more than half of healthcare spending in the province (see Chart 1).
Chart 1. Distribution of Ontario’s population and associated healthcare spending
ONTARIO, 2017
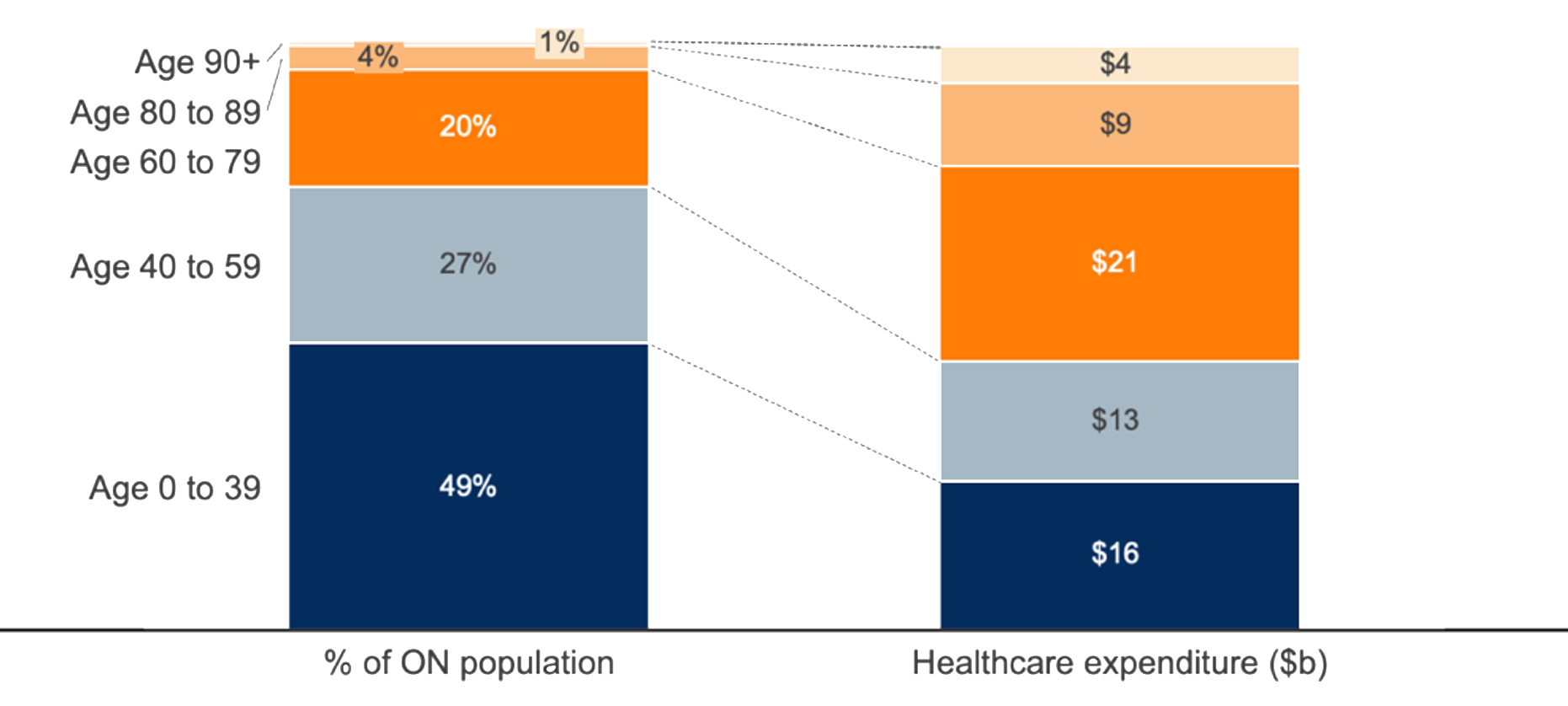
Note: National spending by age group data applied to Ontario population figures.
Source: Fraser Institute
Despite higher spending in these age groups, our healthcare system has been failing our senior citizens. We are seeing unnecessary suffering and premature deaths among our senior population.
These effects are symptomatic of a healthcare system that is overburdened in several areas. Long wait times have plagued Ontario hospitals. At the Ottawa Hospital’s General Campus, only 13% of women waiting for a breast cancer procedure will receive their surgery within the target time. More patients are also left without access to a primary care physician. According to the Ontario College of Family Physicians, one in five Ontarians could be without a family doctor by 2025.
As we age, the impact of these shortcomings intensifies, as illustrated by the increasing occurrence of preventable ER visits (see Chart 2). Without easily accessible services, more and more people end up needing emergency hospital care later in life, and this in turn further exacerbates the pressures on our system.
Chart 2. Potentially preventable emergency department visits in Ontario
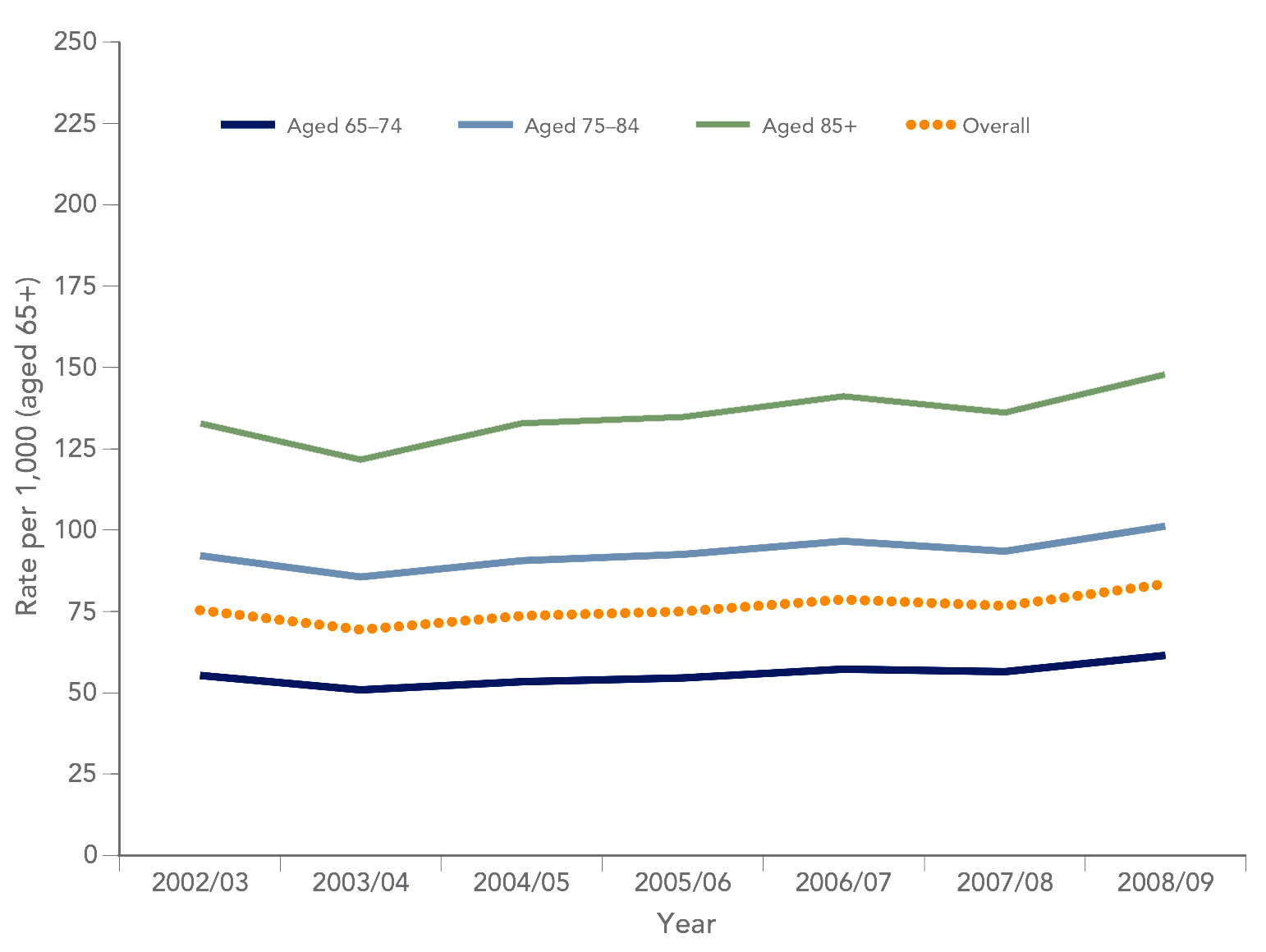
Source: Aging in Ontario: An ICES Chartbook of Health Service Use by Older Adults
Where can we look for solutions?
As strains on our healthcare system continue to grow, the question of how to improve care for more Ontarians has long been at the forefront of public discussion. However, the bulk of this discourse tends to exclude some important issues, and focuses more on a subset of high-profile issues, namely:
- Excessive wait times in ERs, for specialist care and for surgeries
- Shortages of nurses and doctors
- Shortages of beds in hospitals
- Lack of access to long-term care homes and assisted living facilities
These are indisputably crucial aspects of our healthcare system that need to be improved. And though they are newsworthy for good reason, we believe there is another critical element that needs and deserves more attention than it receives: innovations in models of care that can help to reduce the demands and burdens on our healthcare system.
Roundtable discussion
In September, we assembled a group of leaders from across the healthcare industry to discuss the challenges and barriers to such innovations in models of care, specifically innovations in the way we deliver care for seniors. We were fortunate to have the participation of some leading thinkers and experts from across Ontario’s public and private healthcare sectors.
Roundtable participants:
Kamal Gautam
Partner, Healthcare, SATOV Consultants
Fredrika Scarth
Harkness Senior Fellow, Commonwealth Fund
Anne Wojtak
Executive Director, East Toronto OHT
Carolyn Gosse
Clinical VP, UHN@Home and Older Adult Strategy
Helen Angus
CEO, AMS Healthcare
Dr. Howard Abrams
Director, OpenLab
Maya Khurana
AVP Group Benefits, Manulife
Dr. Sid Feldman
Division Head (Care for the Elderly), DCFM
Stephen Goldsmith
VP Business Development, PetalMD
Dr. Vipan Nikore
Founder and CEO, HomeCare Hub
Will Falk
Senior Fellow, CD Howe Institute
To understand and be able to reflect on the barriers we face in Ontario when it comes to developing new models of senior care, we need to expand our definition of what it means to provide care beyond conventional medical settings and approaches.
The vast majority of the attention and healthcare funding dollars in Ontario are focused on institutions, end of life care, and physician care, but there are other forms of care that can help reduce the load on our system. These other forms focus on prevention and de-emphasize our dependence on institutions alone (see Image 1 below).
At our roundtable, the group discussed three categories of care using several emerging programs from around the world within each category to illustrate the kinds of innovations we should be encouraging here at home – innovations that, at scale, could make a real difference. The three categories of care we covered were:
- Preventative care and healthy behaviours
- Multi-disciplinary and integrated care teams for chronic management
- Episodic acute care outside the hospital setting
Image 1. Categories of care discussed at roundtable event
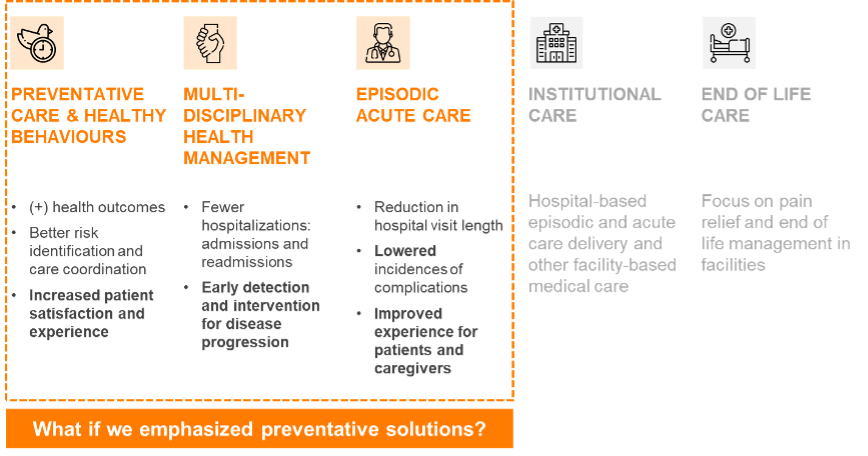
Exploring solutions in three categories of care
1. Preventative care and healthy behaviours
Maintaining healthy behaviours as people enter old age and throughout their old age can enable seniors to reduce the risks of chronic and acute illnesses, while increasing their lifespan and quality of life.
The most successful programs seen in Europe and the US are based on the premise that building a community of peers for seniors leads to greater engagement and improved outcomes.
Peer support and engagement have been shown to increase annual preventative care visits by 23% and reduce ER visits, in some examples by up to 45%. This means improved long-term health and increased satisfaction and happiness on the part of the individuals.
2. Multi-disciplinary and integrated care teams for chronic management
For seniors with more complex needs, a team-based, integrated approach to providing health and social care can dramatically improve outcomes.
This kind of approach helps to prioritize patient-centred care, facilitates better care coordination, reduces unplanned acute care episodes, and improves satisfaction both on the part of patients and healthcare workers.
One team-based model in the US, ConcertoCare, integrates primary, home, and social care for seniors, and has demonstrated reductions in general admissions by 47%, in readmissions by 40%, and in ER visits by 16%.
Ontario’s Family Health Team (FHT) model was a positive step toward this approach. This model allows patients to receive health care under the coordination of an Ontario Health Team (OHT), with teams including primary care physicians, nurses, nurse practitioners, pharmacists, counsellors, health educators, and dieticians providing coordinated care.
The OHT model could and should be the next step toward connecting health and social care for seniors living with chronic conditions.
To make real progress on multi-disciplinary and integrated care, health care organizations and providers need to be supported with payment models that align incentives across provider groups and enable patient-centred care.
3. Episodic Acute Care outside the hospital setting
When seniors do need acute care, they don’t always need to get it in the hospital setting. Yet in Ontario, one in six hospital beds is occupied by a patient who no longer requires hospital procedures or care, but cannot go home safely without clinical supports.
Hospital-at-home programs, which allow patients to receive acute care in their homes, are becoming more prevalent around the world. These programs have demonstrated excellent outcomes, with a 26% lower risk of long-term care readmission, a reduction in hospital bed days from 4.9 to 3.2, a reduction in incidents of delirium from 24% in-hospital to 9% at home, and a reduction in cost of care of between 19% and 30%.
University Health Network (UHN), a hospital network in Toronto, experimented with a hospital-at-home program, but it was cancelled, despite strong results. The dissolution came at least partly because our current healthcare funding model does not offer incentives to deliver acute care outside the hospital setting.
Barriers to innovations
While there have been pilots and experiments in these areas, they have not gained as much traction here in Ontario as programs have in other jurisdictions.
In reviewing the international programs mentioned above, as well as others, the group identified two key barriers in Ontario that hinder the spread and scaling of new innovative models of caring for our seniors:
1. Funding model disincentives
Our current healthcare funding models are largely tied to services delivered in specific settings, and by a narrow set of defined professions. Funding is generally related to the volume of services provided, rather than the outcomes achieved for patients.
These parameters can hinder the scaling of new models of care, because the payment models reinforce silos of care. The majority of our healthcare dollars are earmarked for hospitals, which in turn are actively disincentivized to support care programs outside of the hospital, as a result of their funding formula.
In exchange for supporting and developing programs outside of the hospital setting, our hospitals are rewarded with new patients filling up the beds they just freed up by moving patients to at-home or other care. But they receive no extra funding to provide for the patients now at home, since those services fall outside of funding restrictions (e.g., services delivered outside hospital setting or by professionals outside of preauthorized fields).
Similarly, neither primary care physicians (with the exception of some primary care physicians working in capitated models) nor hospitals realize any economic benefit from preventative care programs.
The current funding environment often prevents care dollars from being spent on non-clinicians, even though such programs are often best delivered by social workers or other caregivers, often in a private sector setting.
2. Bureaucratic hurdles
Our healthcare system is rife with rules and regulations that make it difficult to launch innovative approaches that necessarily require testing and learning.
As an example, we too rigidly adhere to the requirement that everyone should have access to the same care options across the province, which impedes the creation and scaling of pilot programs in a targeted way.
In the US, the Centers for Medicare and Medicaid Services (CMS), the federal agency that is responsible for setting the rules around care for seniors and low-income individuals at a national level, has implemented a policy waiver program that allows state-level agencies to apply for exemptions from certain rules to allow them to create programs that target their local populations’ needs more directly.
Here in Ontario, a similar “local” waiver program would allow municipalities and healthcare organizations to fund the creation of new models of care that meet the needs of their residents, without the requirement to immediately make these programs available across the province.
This is just one of many examples of the rules we have built in our healthcare system that create challenges to building new approaches to solve old problems.
The road ahead
Our healthcare system is in desperate need of reform, and that can’t be done using our traditional methods of “more money for the same kinds of services.” In Ontario, we are blessed with lots of smart, committed entrepreneurs, innovators, and incubators who are continually dreaming up new ideas to improve the delivery of healthcare. But too many of our entrepreneurs are forced to look abroad when they’ve proven a new model and need to commercialize it. We need our best minds to be creating innovative new solutions that can realistically be deployed here in Ontario, and not just exported to the US or other countries to help their residents, but not ours.
We need to do more to support them, including addressing some procedural and policy changes, and providing a viable path forward during the commercialization stage. This will require government to be part of the solution, by pulling innovations into the system with the direct funding of new models.
If we are to support innovation in our healthcare system, we will need to address the systemic barriers that prevent our entrepreneurs and private sector companies from working with our public sector to create and scale new approaches to delivering care.
Our healthcare system has proven itself capable of moving quickly when the need arises, as shown with the rapid response to the COVID pandemic in 2020 and 2021. We need a similar sense of urgency and commitment to change when it comes to reforming policy and payment models to support new models of care delivery for our seniors.
Over the coming months, we will explore possible solutions to these barriers with this group of industry experts, and we invite you to join the conversation. Please contact Kamal Gautam at kamal.gautam@satovconsultants.com if you would like to participate in this important discussion.
